PTSD from abuse can disrupt daily life, relationships, and emotional well-being. Survivors often face intense emotions, hypervigilance, isolation, and harmful coping methods like avoidance or substance use. However, recovery is possible with the right tools and support.
Key strategies include:
- Grounding techniques: Use methods like the 5-4-3-2-1 exercise, deep breathing, or progressive muscle relaxation to manage overwhelming emotions.
- Building a support network: Connect with trusted individuals or support groups to reduce isolation.
- Therapy options: Trauma-focused therapies like CBT, EMDR, and DBT offer structured ways to heal.
- Self-help tools: Apps like Anxiety Journal help track symptoms and triggers for better self-awareness.
If symptoms persist or worsen, professional help is essential. Healing takes time, but small, consistent steps can lead to significant progress.
Understanding PTSD: Effective Coping Mechanisms for Recovery
Common Problems Faced by Abuse Survivors with PTSD
Living with PTSD after experiencing abuse can create a maze of challenges that affect nearly every aspect of daily life. These struggles often overlap, making the path to recovery feel overwhelming. Recognizing these common issues is a key step toward understanding how to manage them and work toward healing.
Trouble Managing Emotions
For many abuse survivors with PTSD, emotions can feel like a rollercoaster that’s impossible to control. Emotional dysregulation – sudden, intense feelings that seem to appear out of nowhere – often stems from the brain’s response to trauma. These emotional shifts, whether they involve numbness, anger, panic, or sadness, are not a reflection of weakness but rather a natural outcome of what the body has endured.
Hypervigilance is another common experience. The nervous system remains in a constant state of alertness, scanning for danger even when none exists. This can lead to exhaustion, difficulty focusing, and being startled by everyday sounds. Sleep often becomes a struggle because the brain refuses to fully relax, leaving survivors perpetually drained.
Feelings of shame and self-blame are also deeply ingrained for many survivors. You might catch yourself thinking, "Why didn’t I fight back?" or "I must have done something to deserve this." These thoughts can spiral into feelings of worthlessness and self-loathing. Even natural reactions like crying or feeling scared may be accompanied by a sense of shame, as if these emotions make you "weak" or "broken."
Anger can be particularly challenging. Survivors often fear that expressing anger might make them resemble their abuser, or they may swing between intense outbursts and complete emotional shutdown. This internal conflict can strain relationships and leave survivors feeling even more isolated.
Feeling Alone and Judged
Social withdrawal is a common response for survivors. While isolating yourself might feel like self-protection, it often deepens feelings of loneliness and depression. The effort required to "put on a brave face" during social interactions can feel overwhelming when you’re already struggling internally.
Past experiences of being dismissed or blamed can make survivors hesitant to share their feelings. This silence often reinforces a sense of isolation.
Trust issues are another hurdle. After being betrayed by someone who was supposed to care for you, it’s natural to question others’ motives. You might find yourself overanalyzing people’s words and actions, constantly searching for signs of danger or deceit. This mental vigilance can be exhausting and may push away those who genuinely want to help.
The stigma and misunderstanding from others can add another layer of pain. Well-meaning friends or family members might say things like, "Just move on", or "It’s all in the past." They may not understand why certain situations trigger you or why recovery isn’t as simple as they assume. This lack of understanding can make you feel even more alienated.
Harmful Coping Methods
In an effort to manage the pain, many survivors turn to avoidance behaviors. You might throw yourself into work, avoid certain places or people, or steer clear of anything that reminds you of the trauma. While avoidance can provide temporary relief, it often limits your life and delays the healing process.
Substance use is another way some survivors attempt to cope. Whether it’s alcohol or misusing medications, substances can dull emotional pain or quiet intrusive thoughts. However, this often comes with the risk of dependency and other health issues.
Self-harm behaviors may develop as a way to manage overwhelming emotions or to combat feelings of numbness. Actions like cutting or burning can provide a fleeting sense of control or release, but they often deepen feelings of shame and self-blame. Similarly, self-sabotage, such as ending relationships or rejecting opportunities, can reinforce negative beliefs about oneself.
Disordered eating is another way survivors try to regain control. Restricting food might create a sense of order in a chaotic world, while binge eating can offer temporary comfort or numbness. Some survivors turn to extreme dieting or over-exercising as a form of self-punishment or to alter their appearance in hopes of preventing future harm.
Engaging in risky behaviors, such as reckless driving or unsafe sexual practices, can stem from feelings of worthlessness or disconnection from one’s own well-being. Survivors often describe a sense of indifference toward their safety, leading to choices that jeopardize their physical and emotional health.
Unfortunately, these harmful coping methods often create a vicious cycle. The temporary relief they provide is followed by guilt, shame, and additional problems, which then drive the need for more unhealthy coping. In the next section, we’ll look at practical ways to replace these patterns with healthier strategies for managing trauma and moving forward.
Helpful Coping Strategies for PTSD
Living with PTSD can feel overwhelming, but there are strategies that can help you navigate the emotional chaos, isolation, and unhealthy habits that often follow trauma. These approaches can empower you to regain a sense of control and start rebuilding your life. Progress may be slow, and setbacks are part of the journey, but every small step counts.
Let’s dive into grounding techniques and mindfulness practices that can help you stay anchored in the present moment.
Grounding and Mindfulness Methods
When emotions spiral or past trauma resurfaces, grounding techniques can bring you back to the here and now. These methods are especially useful during flashbacks, panic attacks, or moments of intense distress.
- 5-4-3-2-1 Technique: This simple exercise can shift your focus from overwhelming thoughts to your immediate environment. Start by identifying five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste. It’s a quick way to reconnect with your surroundings.
- Progressive Muscle Relaxation: Trauma often leaves physical tension in the body. To ease this, tense and then relax each muscle group, starting at your toes and working up to your head. Hold the tension for five seconds before releasing it, and notice the difference. This practice not only reduces stress but also helps you tune into your body’s responses.
- Deep Breathing Exercises: When your body is in fight-or-flight mode, controlled breathing can help calm your nervous system. Try the 4-7-8 technique: inhale for 4 counts, hold for 7, and exhale for 8. This can help counteract feelings of hypervigilance.
- Mindfulness Meditation: Even a few minutes of focused breathing can make a difference. Apps and guided meditations are great starting points, but mindfulness can also be practiced during everyday activities like walking or washing dishes. The goal is to gently redirect your focus when your mind drifts to traumatic memories.
- Cold Water Therapy: A splash of cold water on your face, holding an ice cube, or even a cold shower can quickly interrupt a panic response and help your body calm down.
Creating a Support Network
After trauma, isolating yourself might feel safer, but building a support network is a vital part of healing. This doesn’t mean you need to share your story with everyone. Instead, focus on connecting with people who make you feel secure and valued.
- Identify Trusted Individuals: Surround yourself with family, friends, or coworkers who listen without judgment and respect your boundaries.
- Join Support Groups: Organizations like the National Center for Victims of Crime offer both in-person and online groups specifically for abuse survivors. These spaces can provide understanding and reduce feelings of shame or loneliness.
- Explore Online Communities: If face-to-face interactions feel overwhelming or local resources are limited, online forums and chat groups can provide support at your own pace. Choose moderated spaces with clear guidelines to ensure a positive environment.
- Set Boundaries: Protect your emotional well-being by deciding how much to share and with whom. It’s okay to step back from relationships that leave you feeling worse – it’s an essential part of self-care.
- Communicate Your Needs: Strengthen supportive relationships by letting others know what helps you feel safe. For instance, you might say, “I appreciate when you check in, but I’d rather not discuss the details of my trauma unless I bring it up.”
Therapy Options
For structured guidance, professional therapy offers a range of approaches tailored to your needs. If one method doesn’t feel right, don’t hesitate to explore others – healing is a personal process.
- Trauma-Focused Cognitive Behavioral Therapy (CBT): This widely researched therapy helps you identify and change negative thought patterns related to your trauma. For example, it can help you challenge beliefs like “I’m not safe anywhere” and replace them with more balanced perspectives. Typically, CBT involves 12-16 sessions and includes exercises to practice new coping skills.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is designed for trauma survivors. During sessions, you’ll recall traumatic memories while following guided eye movements or other forms of bilateral stimulation. This helps your brain reprocess the memories so they feel less overwhelming, without requiring extensive verbal recounting.
- Dialectical Behavior Therapy (DBT): DBT focuses on practical skills for managing intense emotions, improving relationships, and handling distress. Techniques include emotion regulation and distress tolerance, which can be particularly helpful if you struggle with self-harm or emotional instability.
- Group Therapy: Combining professional guidance with peer support, group therapy allows you to learn from others’ experiences while practicing new skills in a safe setting. Many find it reduces feelings of isolation and offers fresh perspectives on healing.
- Somatic Therapies: Recognizing that trauma is stored in the body as well as the mind, somatic therapies like body-based practices or somatic experiencing focus on releasing physical tension. These approaches often involve gentle movement, breathing exercises, and heightened awareness of your body.
When choosing a therapist, look for someone with specific training in trauma and experience working with abuse survivors. A strong therapeutic relationship is key to effective treatment.
Finally, consider tools like the Anxiety Journal app to track your symptoms, triggers, and stress levels. Keeping a detailed log can provide valuable insights for both you and your therapist, helping to make your treatment more focused and effective.
sbb-itb-b1dedcc
Using Tools and Resources for Support
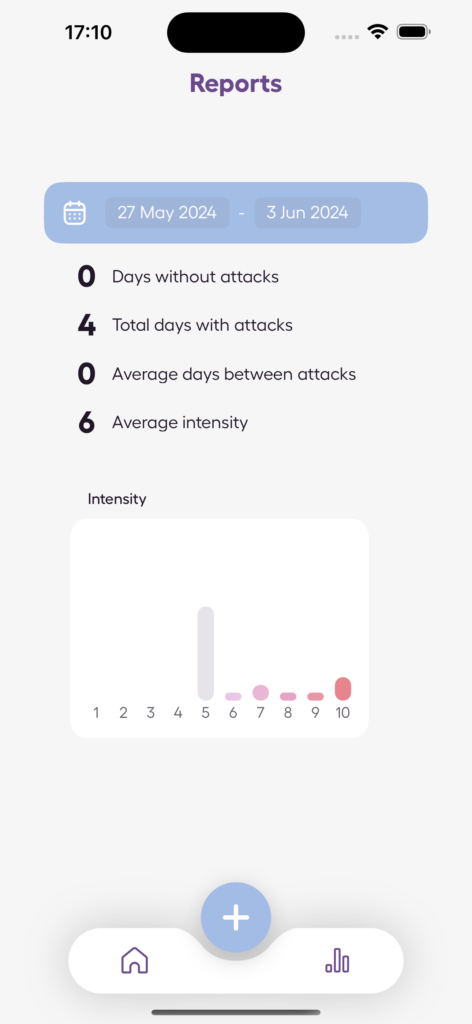
Managing PTSD effectively often involves using tools that help track triggers, monitor progress, and uncover patterns. Digital resources can be a great addition to therapy sessions, offering valuable insights for both you and your mental health professionals. Let’s explore how tools like the Anxiety Journal app can support your recovery journey.
Using the Anxiety Journal App
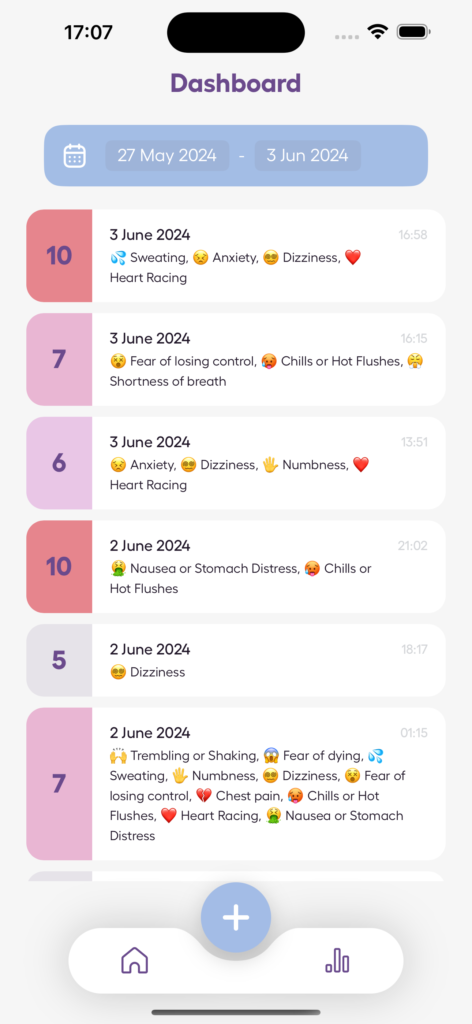
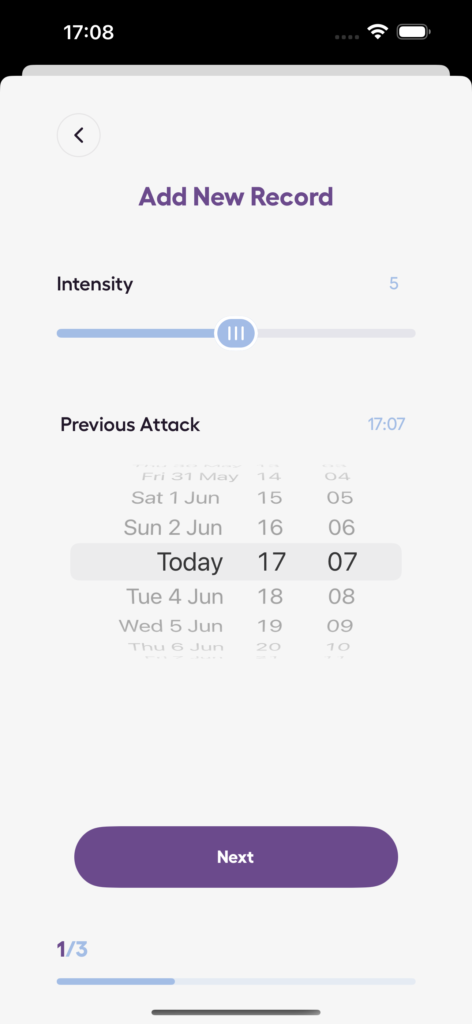
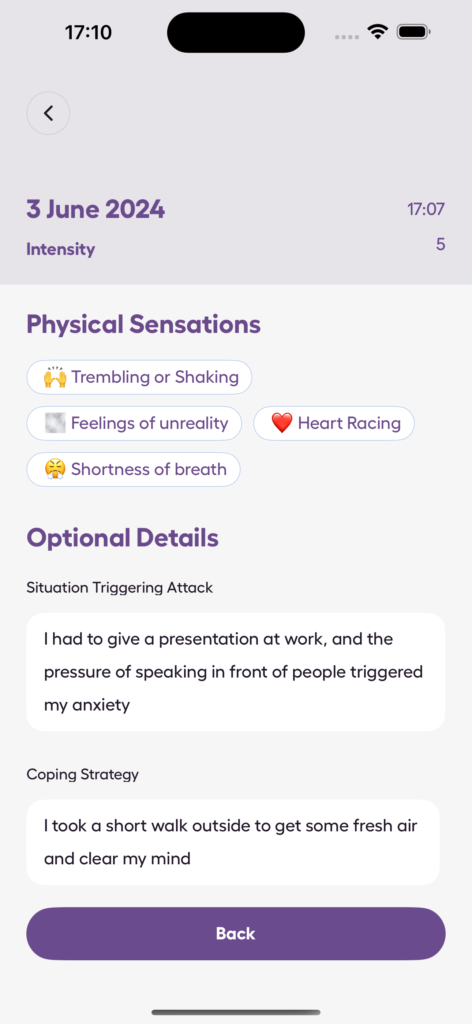
The Anxiety Journal app is designed to help you document and understand your mental health experiences. Acting as both a panic attack and anxiety tracker, it allows you to log entries whenever symptoms arise, creating a detailed record of your emotional state.
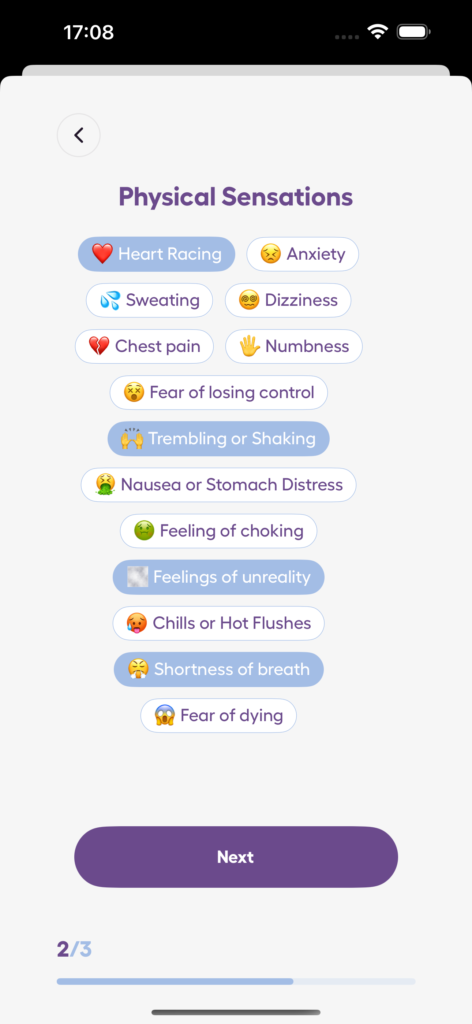
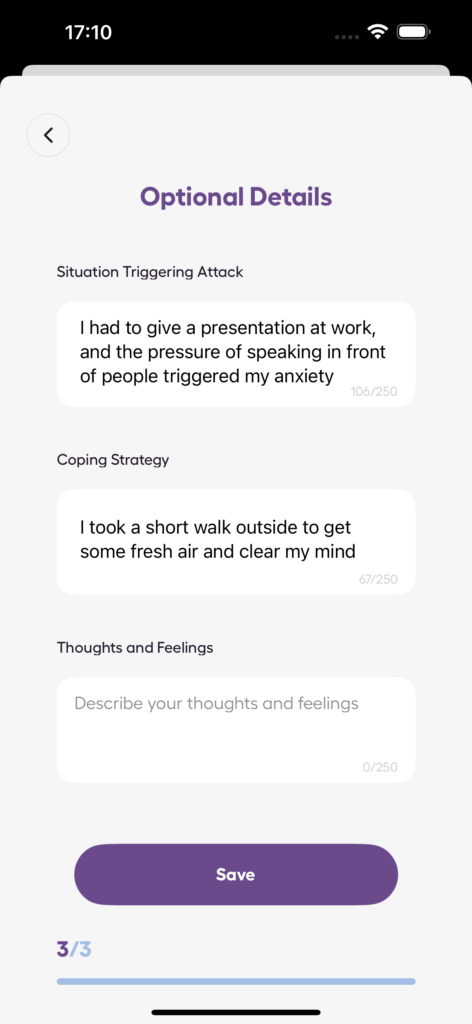
One of the standout features is the attack log, which is especially helpful for those dealing with panic attacks or anxiety episodes. You can record details like potential triggers, physical symptoms, and how long the episode lasted. This kind of information is incredibly useful for identifying patterns and working with therapists to develop effective coping strategies.
Another key feature is stress level tracking, which helps you monitor daily changes in your emotional well-being. By identifying links between specific events, environments, or thoughts and your symptoms, you can gain a clearer understanding of what affects you most. Importantly, the app prioritizes data security, so you can record your experiences honestly without worrying about privacy. Over time, viewing your progress in one place can be a powerful reminder that healing is happening, even if the day-to-day changes feel small.
These features work hand-in-hand with other self-help strategies, offering real-time support when you need it most.
How Self-Help Tools Help
In addition to therapy and grounding techniques, self-help tools provide continuous, personalized support. Apps like Anxiety Journal allow you to capture emotions and symptoms as they happen, removing the need to rely on memory later.
Privacy is another significant advantage. Many tools give you the option to save your progress locally, such as exporting entries as a PDF, so you retain full control over your sensitive information. This can encourage more honest and detailed tracking, which is vital for understanding your journey.
Unlike therapy sessions, which are scheduled, self-help tools are available anytime. Many apps also include evidence-based resources like guided relaxation exercises, breathing techniques, and grounding strategies, giving you immediate access to coping methods when symptoms strike.
Perhaps the most empowering aspect of self-help tools is their adaptability. Since everyone’s recovery process is different, having access to a variety of coping strategies – and the ability to tailor them to your preferences – can make a big difference. The key is to find tools that feel supportive and manageable, helping you take an active role in your healing while maintaining the privacy and control that are so essential after trauma.
When to Get Professional Help
Self-help strategies can be effective for managing mild PTSD, but there are times when professional support becomes essential. If your symptoms persist or worsen despite your best efforts, it might be time to consider reaching out to a mental health professional.
Warning Signs You Need Professional Support
While self-help methods can work well for mild-to-moderate PTSD, there are clear signs that indicate it’s time to seek professional assistance. If you’re dealing with persistent symptoms like frequent nightmares, uncontrollable anger, or severe difficulty concentrating, even after consistent self-help efforts, it’s a strong signal to consult a mental health professional or your primary care provider.
If you’re experiencing feelings of despair, suicidal thoughts, or overwhelming emotional distress, immediate action is critical – contact emergency services right away. Similarly, if you notice harmful coping mechanisms, such as turning to alcohol, drugs, or self-harm, it’s essential to get additional support.
When PTSD begins to interfere with your relationships, work, or daily responsibilities, it’s a sign that specialized treatment is necessary. Additionally, if you’re struggling to manage trauma memories or feel unsure about how to process your experiences, a trained professional can provide the guidance and support you need.
How Mental Health Professionals Can Help
Mental health professionals offer expertise and evidence-based treatments that go beyond what self-help tools can provide. Therapists and counselors specialize in trauma-focused therapies like Cognitive Processing Therapy (CPT), Prolonged Exposure Therapy, and Eye Movement Desensitization and Reprocessing (EMDR). Psychiatrists, on the other hand, can evaluate whether medication might help manage severe symptoms such as depression, anxiety, or sleep issues, potentially enhancing the effectiveness of other treatments.
Professional therapy also offers a safe and structured environment to work through traumatic memories. Therapists can guide you at a pace that feels manageable, helping you create a personalized treatment plan. This plan might include options like group therapy for peer support, family therapy to address relationship dynamics, or targeted approaches for specific symptoms like panic attacks.
If your trauma is tied to an ongoing dangerous situation, mental health professionals can assist with safety planning. They can connect you with resources such as local law enforcement, domestic violence support services, or legal advocacy to ensure your safety.
Conclusion: Moving Forward with Hope
Recovering from PTSD is a journey that requires time, patience, and the right tools. Along the way, it’s completely normal to experience a mix of good days and harder ones – both are part of the process.
The coping strategies we’ve discussed – like grounding exercises, mindfulness techniques, and leaning on support networks – are most effective when practiced regularly and tailored to fit your personal needs. Every small step counts, whether it’s dedicating five minutes to deep breathing, confiding in a trusted friend, or keeping track of your anxiety levels.
It’s important to understand that self-help methods and professional support can work hand in hand. Seeking therapy or psychiatric care isn’t a sign of weakness; it’s a courageous step toward healing and self-awareness.
The goal is to find what resonates with you and remain flexible as your needs evolve over time.
Create a toolkit of strategies to rely on during tough moments. This might include grounding techniques that work for you, a list of people you can reach out to, professional resources, or even apps and tools that help you stay on track. This toolkit not only supports your progress but also gives you the confidence to handle future challenges.
Recovery is achievable. By consistently applying these strategies, you can take back control and move toward a healthier, more empowered future.
FAQs
How can PTSD survivors manage hypervigilance and improve their sleep quality?
Managing hypervigilance and improving sleep quality for PTSD survivors often requires a mix of approaches tailored to individual needs. One effective method is Cognitive Behavioral Therapy for Insomnia (CBT-I), which targets the negative thought patterns and habits that interfere with restful sleep. Establishing a regular bedtime routine and creating a soothing sleep environment – think a cool, dark, and quiet room – can also play a key role in improving sleep quality.
Relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or guided imagery, can help ease hypervigilance and encourage a sense of calm before bedtime. For more severe cases, medications like prazosin may be prescribed to address intense sleep disturbances linked to PTSD. By combining these strategies, many individuals experience gradual improvements in both sleep and overall anxiety levels.
What are healthy coping strategies for PTSD, and how can I move away from harmful ones?
Healthy ways to cope with PTSD include practices like mindfulness, deep breathing exercises, journaling, staying physically active, and leaning on social support. These activities not only help manage stress but also promote emotional balance. On the flip side, turning to harmful coping mechanisms – such as substance use, avoidance, or withdrawing from others – can make symptoms more difficult to manage over time.
Shifting toward healthier habits begins with recognizing patterns of unhelpful behaviors and gradually replacing them with positive actions. Having a support network of trusted friends, family members, or professionals can make this shift feel less overwhelming. Therapy is another powerful resource, offering tools and guidance to address deeper issues while helping you build lasting coping skills. The key is to focus on small, consistent steps – these can lead to real progress over time.
How do I choose the right therapist for trauma-focused therapy, and how can I tell if their approach works for me?
When choosing a therapist who specializes in trauma, it’s essential to find someone experienced in addressing trauma and PTSD. They should use proven therapeutic methods and foster a safe, welcoming space where you feel at ease opening up. During an initial consultation, don’t hesitate to ask about their approach and techniques.
To figure out if their style of therapy suits you, think about how well it matches your goals and personal needs. Attending a few sessions can give you a sense of whether their methods click with you and if you’re noticing progress. Trust your gut – feeling genuinely understood and supported is crucial for therapy to work effectively.