Living with chronic pain and anxiety often feels like being stuck in an endless loop – pain triggers anxiety, and anxiety worsens pain. But the cycle can be interrupted. Here’s how:
- Chronic Pain Defined: Pain lasting over 3-6 months alters how the brain processes pain, increasing vulnerability to anxiety.
- Anxiety’s Role: Anxiety amplifies pain through stress hormones, inflammation, and heightened sensitivity. It also leads to muscle tension and negative thought patterns.
- Daily Impact: This cycle disrupts sleep, relationships, work, and physical activity, compounding the problem.
Key Strategies to Break the Cycle:
- Mental Health Tools:
- Cognitive Behavioral Therapy (CBT): Reframes negative thoughts and reduces avoidance behaviors.
- Mindfulness: Teaches acceptance of pain and anxiety, reducing emotional distress.
- Journaling: Identifies triggers and tracks progress for better symptom management.
- Lifestyle Adjustments:
- Exercise: Activities like walking, yoga, or swimming ease pain and improve mood.
- Nutrition: Anti-inflammatory foods (e.g., salmon, walnuts) help stabilize mood and reduce pain.
- Sleep: Consistent routines and habits improve rest and emotional resilience.
- Medical and Alternative Treatments:
- Medications like antidepressants, anticonvulsants, or nerve blocks may offer relief.
- Therapies like acupuncture, massage, and physical therapy address both pain and anxiety.
- Tracking and Routine:
- Use tools to monitor symptoms and build consistent daily habits for stability.
Breaking free requires a mix of mental, physical, and medical approaches. Start small – track symptoms, practice mindfulness, or take a short walk. Each step helps you regain control.
Anxiety Regulation to Reduce Chronic Pain – Pain Reprocessing Therapy with Alan Gordon, LCSW
Mental Health Strategies to Break the Cycle
Breaking free from the pain-anxiety cycle requires focused mental health strategies that address both issues together. These proven approaches can help you take control of your thoughts, emotions, and physical reactions.
Cognitive Behavioral Therapy (CBT)
CBT is widely regarded as one of the most effective ways to manage both chronic pain and anxiety. This therapy zeroes in on identifying and changing negative thought patterns that perpetuate the cycle. For instance, when you’re dealing with chronic pain, it’s easy to slip into catastrophic thinking, like "This pain will never go away" or "I’m completely powerless."
CBT helps you reframe these thoughts. Instead of "I can’t handle this pain", you learn to think, "This is challenging, but I have tools to manage it." This mental shift influences how your brain interprets pain signals, making them less overwhelming.
The therapy also incorporates behavioral techniques, encouraging you to gradually resume activities you may have avoided due to pain or anxiety. This process not only builds confidence but also reduces fear-driven avoidance behaviors.
Studies consistently show that CBT can lower both pain severity and anxiety levels in individuals with chronic conditions. The skills you develop during therapy often remain useful long after your sessions end, making it a valuable step toward long-term relief.
In addition to changing thought patterns, other mental health tools can help ease physical tension and promote mindfulness.
Mindfulness and Relaxation Methods
Mindfulness-based practices offer a practical way to disrupt the pain-anxiety cycle by altering how you relate to these experiences. Mindfulness-Based Stress Reduction (MBSR) has shown particular success for individuals coping with chronic pain and anxiety.
The idea is to observe pain and anxiety without reacting impulsively. Instead of resisting pain or spiraling into worry, mindfulness teaches you to acknowledge these sensations with acceptance. By doing so, you can reduce the extra suffering caused by fighting against what you’re feeling.
Relaxation techniques like progressive muscle relaxation or deep breathing exercises, such as the 4-7-8 method, can help release physical tension and activate your body’s calming mechanisms.
Daily meditation also plays a role in enhancing emotional regulation and altering how you perceive discomfort. Over time, it helps you develop a steadier, more composed response to pain and anxiety.
When paired with consistent progress tracking, these approaches form a strong foundation for breaking the cycle.
How Journaling Helps Manage Anxiety
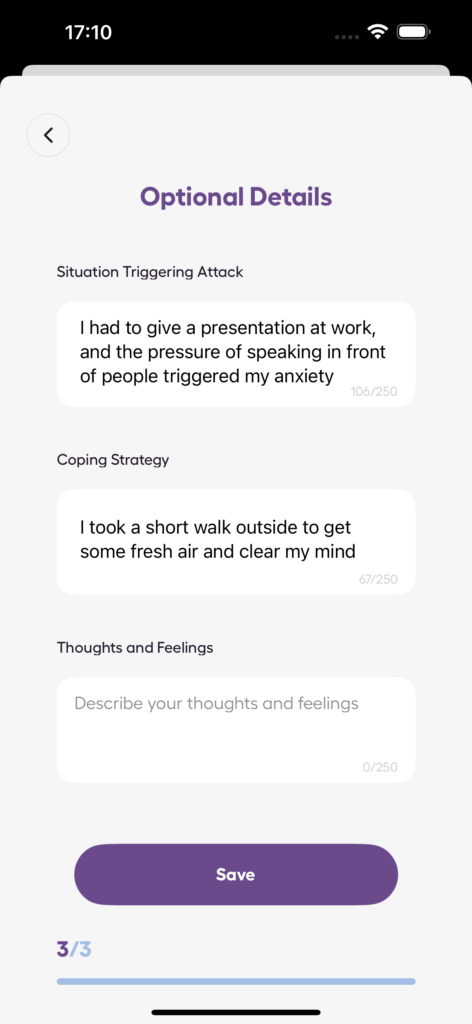
Journaling is another effective tool for managing anxiety, as it helps you uncover triggers and patterns. For example, you might notice that your anxiety intensifies at specific times of day, during certain activities, or when your pain worsens.
Writing down your experiences creates a sense of distance from anxious thoughts, giving you clarity. You begin to see patterns in your anxiety – when it spikes, what triggers it, and how it interacts with your pain.
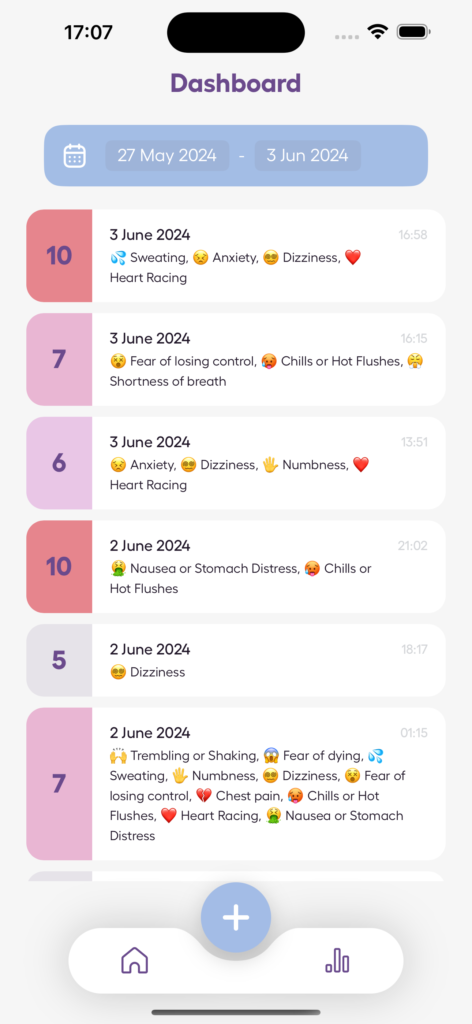
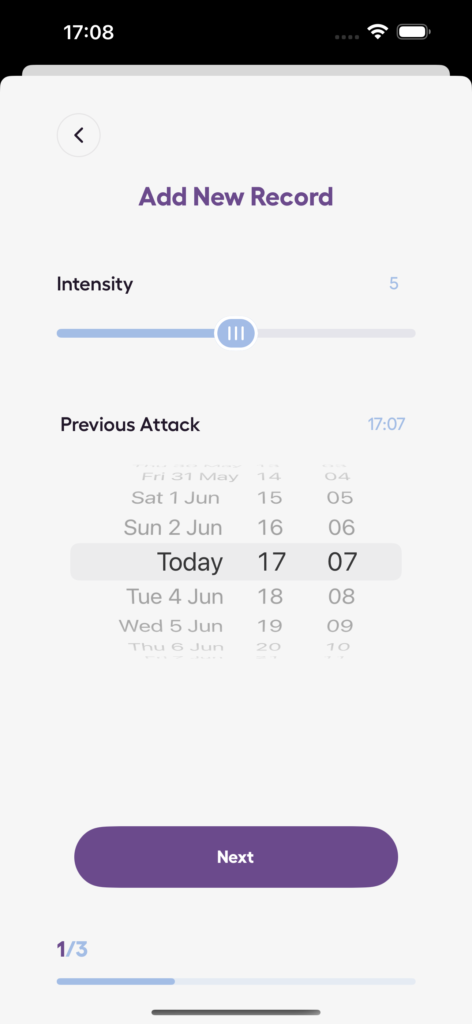
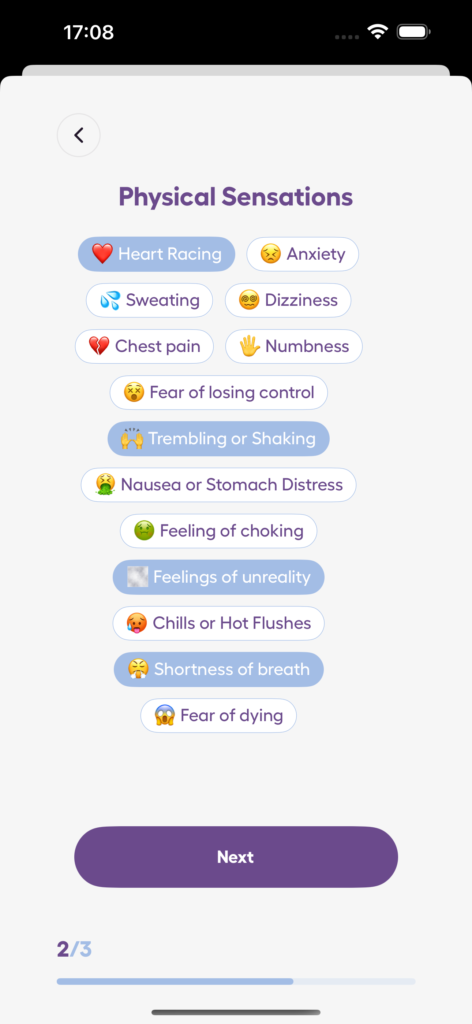
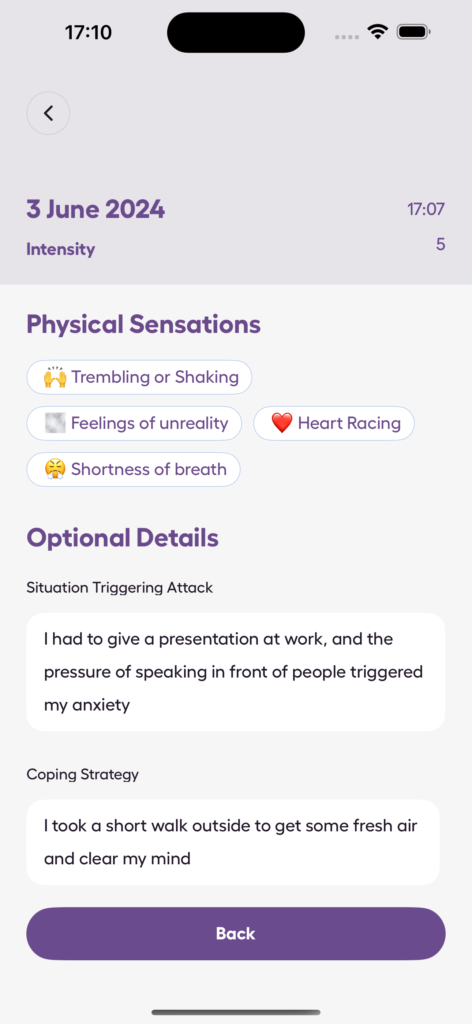
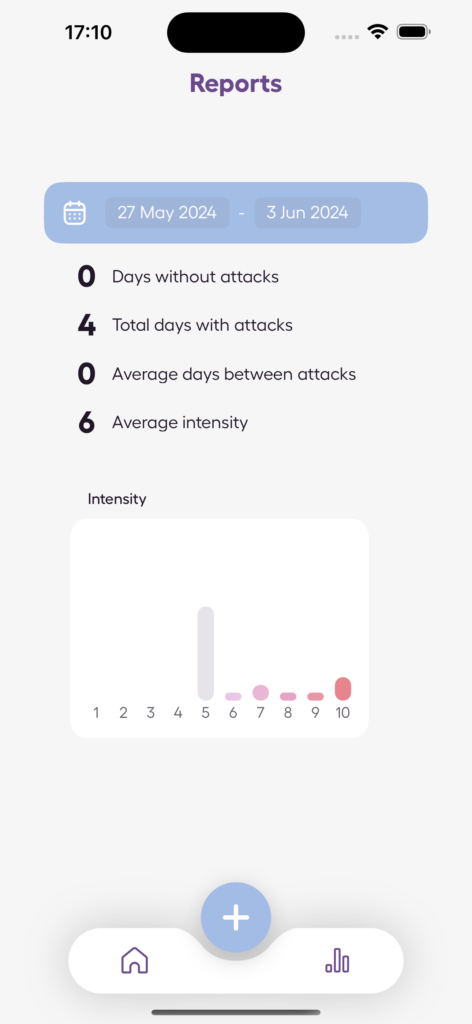
Apps like the Anxiety Journal can make this process even easier. They offer features like detailed logs and stress level tracking, allowing you to document your symptoms in real-time. Over time, these records can reveal trends that might not be obvious in the moment. Plus, seeing your progress through the data can be incredibly encouraging as you work to manage chronic conditions.
Journaling also provides a private outlet for emotions you might not feel ready to share with others. Writing can help you process difficult feelings constructively, reducing the emotional weight of both pain and anxiety.
The insights you gain from consistent journaling can also be a valuable resource for your healthcare team. By presenting clear patterns in your symptoms, you empower your providers to make better-informed decisions about your treatment plan. This collaborative approach reinforces your role in breaking the pain-anxiety cycle, giving you a sense of control over your journey.
Physical and Lifestyle Changes for Pain and Anxiety Relief
While mental health strategies lay the groundwork for breaking the pain-anxiety cycle, physical and lifestyle adjustments can help reinforce recovery. These practical changes work hand-in-hand with mental health efforts to ease chronic pain and reduce anxiety.
The Role of Regular Exercise
Engaging in low-impact exercise can ease pain and lift your mood. The key is to find activities that are gentle on your body yet still effective.
Walking is a simple, accessible option for many people dealing with chronic pain. Even a quick 10-minute walk can trigger the release of endorphins – your body’s natural pain relievers and mood enhancers. Start small and gradually increase your distance as your body adjusts.
Yoga is another excellent choice, blending gentle movements with breath control and mindfulness. This combination can ease muscle tension and calm your nervous system. Many beginner-friendly yoga classes are available, making it easy to get started.
Swimming offers resistance training without stressing your joints. The buoyancy of water supports your weight, enabling more freedom of movement compared to land-based exercises. Even walking in a shallow pool can provide similar benefits.
Research supports the benefits of regular exercise for those with chronic pain conditions like fibromyalgia and back pain, showing significant reductions in both pain and anxiety symptoms.
The Centers for Disease Control and Prevention (CDC) suggests aiming for 150 minutes of moderate exercise per week, but this can be broken into smaller, manageable sessions. Even 15 minutes of light activity a few times a week can start to make a difference in how you feel, both physically and emotionally.
To complement exercise, focusing on proper nutrition and sleep can further boost your overall well-being.
Nutrition and Sleep: A Vital Connection
What you eat and how well you sleep play a major role in managing pain and anxiety. Poor sleep can heighten pain sensitivity and emotional distress, creating a vicious cycle that disrupts rest even further.
Incorporating anti-inflammatory foods into your diet can help. Think fruits, vegetables, whole grains, and omega-3-rich options like salmon, walnuts, and flaxseeds. These foods support your body’s natural healing and can help stabilize your mood.
At the same time, cutting back on processed foods, added sugars, and excessive caffeine can prevent pain flare-ups and mood swings. These items can contribute to inflammation and energy crashes, worsening both physical and emotional symptoms. Instead of making drastic changes, try gradual swaps – like replacing sugary snacks with fresh fruit or trading one cup of coffee for herbal tea.
Sleep quality is equally important. Poor sleep lowers your pain threshold, making discomfort feel more intense while also reducing your emotional resilience. Establishing a consistent sleep routine can signal to your body that it’s time to wind down and recover.
Simple steps for better sleep include sticking to the same bedtime and wake-up time daily, even on weekends. Keep your bedroom cool and dark – around 65–68°F is ideal – and avoid screens for at least an hour before bed to limit blue light exposure, which can interfere with sleep hormones.
Staying hydrated and eating regular meals throughout the day also helps maintain stable energy levels and emotional balance. Dehydration and skipped meals can lead to blood sugar dips, which may trigger stress and worsen symptoms.
Building Daily Routines for Stability
Having a consistent daily routine can reduce anxiety and help you manage pain more effectively. Structure and predictability create a sense of control, which can feel empowering when dealing with chronic conditions.
Start by setting regular times for meals, exercise, and relaxation. You don’t need to plan every minute of your day, but having key anchor points can provide stability. For example, you might take a short walk after breakfast, eat lunch at the same time, and unwind with gentle stretching before bed.
Pacing your activities is crucial. Instead of overexerting yourself on high-pain days or avoiding activity altogether on low-pain days, aim for a steady level of activity. Break larger tasks into smaller, manageable steps with rest periods in between.
Flexibility is also important. On days when pain levels are higher, adjust your routine rather than abandoning it completely. If your usual 20-minute walk feels overwhelming, try a brief 5-minute stretch instead. Small adjustments still contribute to maintaining your routine.
Tools like the Anxiety Journal app can help you track your activities, anxiety levels, and progress, giving you a clearer sense of control over your symptoms.
Involving friends or family in your routine can boost accountability and motivation. Whether it’s a walking buddy, someone to share meal prep duties, or simply a check-in partner, social support makes it easier to stick with healthy habits during tough times.
sbb-itb-b1dedcc
Medical and Alternative Treatments
When lifestyle changes and mental health strategies don’t fully address chronic pain and anxiety, medical treatments and alternative therapies can offer additional relief. Collaborating with healthcare professionals to find the right combination of treatments often leads to better outcomes than relying on a single approach.
Medical Treatment Options
Some medications can target both chronic pain and anxiety, making them especially helpful for disrupting the pain-anxiety cycle.
Antidepressants are often the first choice for treating both conditions. SNRIs like duloxetine (Cymbalta) and venlafaxine (Effexor) are approved for generalized anxiety disorder and are also effective for chronic pain conditions such as fibromyalgia and diabetic neuropathy. These medications work by increasing serotonin and norepinephrine levels, which can improve mood and reduce pain.
Tricyclic antidepressants like amitriptyline and nortriptyline are another option. They not only help with pain relief but also improve sleep and reduce anxiety symptoms.
Anticonvulsants are another promising category. For example, pregabalin (Lyrica) is effective in treating nerve pain and conditions like generalized anxiety and social phobia. Similarly, gabapentin (Neurontin) has been shown to help manage both chronic pain and social anxiety. These medications calm overactive nerve signals, which can ease both physical and emotional symptoms.
Benzodiazepines (such as lorazepam or alprazolam) may be prescribed for short-term relief of acute anxiety episodes. However, due to their potential for addiction and tolerance, they are typically used under close supervision and for limited periods.
Opioid medications can provide relief for severe pain but come with significant risks, including dependence and increased pain sensitivity over time (a condition known as opioid-induced hyperalgesia). They are rarely used alone and are most effective as part of a broader treatment plan.
For targeted pain relief, procedures like nerve blocks or epidural injections can help reduce pain at its source, which may also alleviate related anxiety.
Alternative Therapy Options
Many people find that alternative therapies complement medical treatments and help address both physical pain and anxiety.
Acupuncture is widely recognized for its ability to relieve chronic pain. By stimulating specific points on the body, acupuncture may trigger the release of natural pain-relieving chemicals, while also promoting relaxation.
Massage therapy provides both physical and emotional benefits. Techniques like Swedish massage or deep tissue massage can ease muscle tension and reduce stress. The human connection and focused attention during a massage can also help interrupt the pain-anxiety cycle.
Chiropractic care focuses on improving spinal alignment and joint function, which can be especially useful for issues like back pain, neck pain, and headaches. Many chiropractors also incorporate stress management techniques and lifestyle advice into their treatments.
Physical therapy combines exercises and hands-on techniques to enhance mobility and reduce pain. Physical therapists also teach strategies for managing physical limitations, which can help reduce anxiety tied to movement or activity.
Meditation and mindfulness practices are powerful tools for managing both pain and anxiety. By changing how you relate to discomfort, these techniques can reduce the emotional strain that often worsens physical symptoms.
Why Team-Based Care Works Best
A team-based approach to treatment often delivers the best results. Chronic pain and anxiety are complex conditions that benefit from the combined expertise of multiple healthcare professionals.
Your primary care physician can oversee your care and manage medications, while a pain specialist may focus on advanced treatments like injections or other interventions. A mental health professional can provide therapy and help with anxiety management, and a physical therapist can address movement and mobility issues.
This collaborative approach ensures that all aspects of your condition are addressed. For instance, a therapist might identify anxiety triggers that exacerbate your pain, while a physical therapist could pinpoint movement patterns contributing to both discomfort and stress.
Good communication between team members is crucial. When healthcare providers share updates about your progress, they can adjust treatments more effectively and avoid conflicting strategies. Pharmacists also play a key role, especially if you’re taking multiple medications. They can monitor for potential interactions and suggest ways to optimize your medication schedule.
The team approach also provides emotional support. If one aspect of your treatment becomes challenging, other team members can offer encouragement or suggest alternatives, helping you stay on track.
Regular team check-ins or shared health records ensure everyone stays informed about your progress. This kind of coordination allows for quicker adjustments when something isn’t working and encourages creative problem-solving when standard treatments fall short.
Tracking Your Progress and Building Strength
Breaking free from the pain–anxiety cycle takes more than just effort – it requires thoughtful strategies and consistent tracking. By keeping tabs on your symptoms, you can uncover patterns and gain insights that are crucial for your recovery.
Using Self-Monitoring Tools
Tracking your symptoms regularly can help you see the connection between chronic pain and anxiety. By noting details like pain intensity (on a scale of 1–10), location, type, and how it ties to anxiety, you can start identifying triggers. These might include physical activity, diet, sleep patterns, weather changes, or even emotional stress [6–8].
Digital tools, such as Anxiety Journal, make this process easier. These apps let you log anxiety levels, panic episodes, and stress patterns over time. They also reduce the chances of forgetting important details and give you real-time data to share with your healthcare provider.
In fact, a 12-week study using a digital pain mapping app demonstrated noticeable shifts in both pain intensity and its overall spread. This shows how regular tracking can uncover trends that might otherwise slip under the radar.
It’s equally important to track emotional factors – like frustration, stress responses, or anxiety episodes. This combined approach helps you see how your emotions influence pain flare-ups. Plus, it equips you to have more meaningful, personalized conversations with your healthcare team.
Once you’ve spotted clear symptom patterns, the next step is building the strength to tackle these challenges head-on.
Building Long-Term Strength and Coping Skills
Tracking is just the start – developing resilience is the key to making lasting progress. Resilience, or your ability to bounce back from setbacks, plays a vital role in breaking the pain–anxiety cycle [10–12]. It’s something you can build over time through self-awareness and consistent effort.
Start by reflecting on your current coping strategies. Which ones help you manage stress or regain emotional balance? From there, expand your toolkit with practices like mindful breathing, gentle physical movement, or cognitive reframing. Building a strong support network – whether through loved ones or support groups – can also provide both practical help and emotional encouragement.
Improving emotional management takes practice. Begin by using coping techniques during calmer moments, then gradually apply them in more challenging situations. This step-by-step approach helps you build confidence in your ability to handle stress.
Creating steady daily routines can further strengthen your resilience. Stick to regular sleep patterns, eat balanced meals, and set aside time for relaxation. These habits create a solid foundation for your recovery. Plus, by actively tracking your progress, you shift from being a passive patient to taking an active role in your healing journey.
The combination of consistent monitoring and a variety of coping skills can help you make meaningful strides in breaking the pain–anxiety cycle.
Conclusion: Breaking the Cycle for a Better Life
Breaking free from the cycle of chronic pain and anxiety is possible with the right mix of approaches. By blending mental health techniques, lifestyle changes, and medical treatments, you can address both issues effectively.
Techniques like Cognitive Behavioral Therapy (CBT) and mindfulness can help you reshape negative thought patterns and manage stress more effectively. These mental tools lay the groundwork for better self-awareness and open the door to meaningful progress, especially when paired with medical care.
The cornerstone of long-term improvement is consistent self-monitoring and awareness. Tools for tracking your anxiety levels, noting panic episodes, and identifying links between emotional states and pain flare-ups can turn vague symptoms into actionable insights. This kind of data empowers you to work with healthcare professionals to create treatment plans tailored to your needs.
Even small actions, like practicing a breathing exercise, going for a short walk, or keeping a symptom journal, can make a big difference. Combining these strategies, staying consistent, and being patient with yourself can help you regain control over your life.
It all starts with those first steps. The cycle can be broken, and a better, more balanced life is within your reach.
FAQs
How does Cognitive Behavioral Therapy (CBT) help break the cycle of chronic pain and anxiety?
Cognitive Behavioral Therapy (CBT) offers a powerful approach to breaking the ongoing cycle of chronic pain and anxiety. It focuses on how thoughts, emotions, and behaviors influence each other, helping individuals recognize and challenge negative thought patterns tied to their pain. This process can reduce emotional distress and build greater mental strength.
CBT also promotes healthier habits, like slowly increasing physical activity and using relaxation techniques. These strategies can help ease the intensity of both pain and anxiety. By shifting the way pain is understood and handled, CBT gives people the tools to take back control and interrupt the cycle of discomfort and distress.
How can I use mindfulness in my daily routine to ease chronic pain and anxiety?
Incorporating mindfulness into your daily routine can be a helpful way to ease the loop of chronic pain and anxiety. Practices like deep breathing, body scans, and guided imagery encourage you to stay in the present moment, helping you approach physical sensations with a calmer, more accepting mindset.
You might also explore activities like walking meditation or simply pacing yourself during daily tasks. These approaches can encourage relaxation, lower stress levels, and gradually strengthen your ability to cope. Even dedicating just a few minutes each day to mindfulness can create noticeable shifts in breaking the pain-anxiety cycle.
How can I track my symptoms to better understand the connection between chronic pain and anxiety?
Tracking your symptoms can be a game-changer when it comes to understanding the connection between chronic pain and anxiety. Start by keeping a journal where you jot down the date, time, pain intensity (using a scale from 0 to 10), and any noticeable changes in how the pain feels. Alongside these details, include notes about possible triggers, your activities, or stress levels to help spot patterns.
If pen and paper aren’t your style, try using a symptom-tracking app. These digital tools make it easier to log your symptoms regularly and even analyze trends over time. The key is consistency – by keeping up with your tracking, you’ll uncover insights into how pain and anxiety influence each other, giving you the knowledge to start breaking the cycle.